Have you been looking for a solution to your back pain for a long time now? Tried everything? Run out of options? Been told to learn to live with it?
I remember not being able to lie flat on my back in my mid 20s. The pain in my back was too much. I didn’t think I’d ever be free of it. Osteopaths, Physio’s, weight training, strengthening, stabilising, stretching, yoga…. What more could I do? 🤷🏻♂️
Back pain is the number one searched health problem in the world. So you aren’t the only one… I know many people have similar thoughts about how to cope with chronic back pain. Chronic is an interesting term, is it not? Is it chronic by virtue of how much it’s a problem, or is it chronic by virtue of time? Chronic pain means long term. Which leads to thoughts such as “will it ever go away?” and amounts to countless and seemingly endless treatments, if not surgery. Despite all of the time you have struggled with it, and all of the treatments you have had on it, have you ever considered that your back may be an outcome of other factors in your body? That is to say that other parts of your body may be contributing to the state of your lower back today.
As for me, a broken jaw, an umbilical hernia, knee surgery, multiple ankle sprains and a dislocated shoulder all went a long way to forcing my skeleton to adapt in a way that began to compromise my lower back. The downgrade in movement potential at one structure compared with its opposite structure served to distort my skeleton over time. There is much information on how this happens in my Instagram feed (@GaryWard_aim).
In essence if my right ankle no longer works like my left ankle, and my left knee no longer works like my right knee, what do you think the outcome at my pelvis might have been? If a pelvis adjusts its resting posture and its movement potential (which it has to) what is the knock on effect to the lower back that sits atop of it and is influenced by the pelvis? Add to this my right shoulder no longer working like my left shoulder and the left side of the jaw now being different to the right side of the jaw, not to mention the subsequent neck impact, how are these higher limitations now going to work down and affect the spine?
Can you see how the lower back gets compromised and caught up in the middle of it all? It’s perhaps not conventional thinking, where we are used to the notion that if my back hurts, I should treat my back, right? Sadly that localised way of thinking doesn’t seem to work out too well for people. A much more global or whole way of looking at the body pays much greater dividends. You have heard the term ‘it’s all connected’ before, well, it turn out it is AND we can track and follow just how connected it is which creates the possibility of better understanding how our back might be being affected by the rest of our body.
To cut a long story short… I found movement and dived so deep into it so I could dig myself out of this seemingly never ending hole. I didn’t feel like anybody could help me and so my journey began to take ownership of it myself
To make this an engaging article I’ll share some key concepts that contributed to my way out of that never ending discomfort. It’s not conventional, so don’t expect to read about massage or exercises… it’s more about how we manage our mass as we move ourselves around the planet.
What I discovered is it’s more about how you hold yourself upright, the potential for movement you have in each part of your body, how each part of your body communicates to another and how it responds to that rich life history of yours: movement comes down to habits and behaviours. Various injuries and adaptations to our movement creates new habits and new behaviours that may not ultimately be useful when it comes to being pain free further down the road of life.
One of the reasons back pain is a highly searched term, is not only because it’s prevalent but also because it’s often not your back that is the culprit; and if you have followed me for long enough, you’ll recognise that that means to treat the back in isolation will not get to the bottom of the problem. If we’re not getting to the bottom of the problem then people will keep searching for answers.
Often back pain is attributed to weak glutes. A large percentage of back pain sufferers will have heard this before and despite profound attempts to strengthen these things up, the back pain persists… Well, we know that weak glutes can be directly attributed to lack of or insufficient motion between the bones and joints where the glutes attach. Sadly strengthening the glutes in a conventional way does not necessarily influence and improve the potential for movement at these joints. So ultimately, the glutes will not change their characteristic behaviour since the permission to do so is simply not there. If joints are limited, muscles cannot do their thing! Somewhere along the line this was omitted from anatomical learnings…
The thing about joints is that for a joint to move freely, it requires the joint adjacent to it to also move freely, which in turn requires the joint adjacent to that one to move freely. Since all joints have adjacent joints, this little theory requires all joints to work perfectly so that each can experience optimum movement – hence the whole body approach versus a localised and isolated approach.
If you want your glutes to work well, so as to relieve your back pain, how many other joints are you paying attention to at the same time? And if we hit the gym and start battering our glutes without making sure other joints are involved in the movement, are we simply wasting our time. Is there anything simpler and more rewarding we could be doing to increase the impact of this approach? My wake up your sleepy glutes approach with Dr. Rangan Chatterjee may give you some insight into this… (there are four videos we put together for his first book, I have linked to the first one)
To break this down a little for you, the glute muscles attach onto your pelvis and femur and are thereby affected by the movement potential at the pelvis and the hip joints. Just above your pelvis is the low back. Can you see how limited movement at the pelvis would directly affect movement at the spine? And how it’s possible that limited spinal motion is a factor for back pain? This is not to say that the glutes are the culprit here… The fact that the glutes aren’t ‘firing’ suggests they are only doing half a job so what is it that is creating a lack of movement potential in the hips/ pelvis that is showing up in the glutes?
Your pelvis is influenced directly by the two legs below it. You can stand up now, rotate your pelvis to the right and notice instantly that there is a change in both feet. In return, a change in either foot will reach up and directly affect the movement at your pelvis. Less obviously but still true, the movement at the pelvis will change how your spine rests as a result of this change. How your pelvis and back have organised as a result of any changes to your lower limbs is one that is individual to the patient. We know your hips and pelvis are connected to your feet and that lack of foot motion correlates with lack of (or excess) motion at the pelvis. Neither lack nor excess can be optimal. You will have heard the term neutral spine as well… but similar to strengthening your glutes, attempts to neutralise your spine without paying attention to pelvic position and its response to your legs and feet, is another wasted effort unless that effort has a positive impact on your foot’s ability to move and subsequent postural adaptation.
We also know your hips and pelvis have a direct relationship with your ribcage which is directly impacted upon by shoulder, scapular and arm limitations as well as skull and neck movements. It’s easy to see how the middle of all this can take the brunt, especially after the injuries to my own extremities that all manifested in my own low back pain.
So, this ‘middle’ of yours? How is it impacted when you stand up and move around? After we have all probably spent years strengthening and stabilising our core to manage this back pain – hasn’t everybody? – it remains to say that the number one search term on Google has something to do with low back pain, in particular L4/L5 disc herniation. Why aren’t we getting better?
Interestingly L4/L5 (lumbar vertebrae 4 and 5) is a pretty accurate description of your own Centre. The location of your body’s centre of mass is just below your naval (which is at L3) placing it just over the area of L4/L5. Why is this important? Well, if your own centre isn’t resting in the centre, then the resting posture of your spine can become altered.
Is back pain linked to my base of support?
I’d like to discuss a relationship you have between your centre of mass (COM) and base of support and ask the simple question, could this be a relevant subject to explore when considering your back pain?

We can then look at its impact on your posture, how you hold yourself, and how that contributes to limiting movement in your lower back. and how that could be relevant to your back pain and point out a few things you can be paying attention to.
In order to stand upright, you simply have one job, and that is to keep your Centre of Mass (COM) over or inside of your Base of Support (BOS). Your BOS is the area on the ground that you can ‘see’ if you were to draw a line around the outside of both feet as you stand naturally.
This is why we check for foot pressures in my Wake Your Body Up programmes. As it does give you an insight into where your centre is. We are interested in where the pressure is that you feel in your feet when you stand as this does give us an idea of exactly how you manage your own centre of mass:
- is it too far forward in the forefeet?
- Is it too far back in the heels?
- Is it too far into the left foot?
- Is it too far into the right foot?
- Is it in the left forefoot and the right heel?
- Is it in the right forefoot and the left heel?
- Or is it “just right?”
Ultimately it’s likely you are a large or small combination of all three pairings here: front/ back; left/right or rotated.
Now picture what happens if you are forwards in your feet, did you notice your pelvis slip forward?. Can you imagine or feel what that does to your low back and that centre point? A change would occur in the sagittal plane (extension) which inevitably begins to close the posterior joints of your spine. Imagine what happens when you carry the majority of weight in your right foot? Can you see that your centre is pulled away from its optimal point to the right? This would illicit a change in the resting shape of the spine in the frontal plane (side bend).
I should mention that if joints are equally open on both sides then the joint space is not compromised, but if the joint space is held more closed than open on one side (for instance if the pressure in your feet stays forward and struggles to come back) then it can become a problem. A long term problem perhaps if the overall resting position of your body is not addressed. These changes of shape that occur as a result of how you hold your mass over your base alters the comfortable resting position of the spinal / intervertebral joints. Opening on one side, closing on the other. Could be left or right, front or back.
What’s important is if the pressure in your feet is not level and you have back pain, then you can assume your resting spinal posture is not as good as you would like it to be.
If you work hard to stabilise and strengthen this postural set up, are you doing anything useful for your back pain? Or would you be better served to focus on how you effortlessly hold and move your centre of mass over your base of support?
This brings me on to another piece of advice that many of us are subjected to. “Stabilise your spine. Strengthen your core”.
The issue of stabilising your spine:
If you only train to stabilise your spine, you can slowly begin to compromise whole body movement. Consider the force plate visual in the image: would you want to stabilise that distribution of your body mass? Or work to reorganise it so that you become more balanced first?
What’s interesting as I mention in my book What The Foot? is that the more we seek to stabilise our spine the more unstable in general our readings when we stand on a force plate become (more movement in cm2 in less time) whereas the more mobile we become throughout our whole body, the more stable we are able to be (less movement in cm2 over more time).
Stable and rigid are in my opinion not the same. Rigid is when you work so hard to make sure something can’t move and stable is attained by effortlessly standing still and enjoying movement without compromise to your balance. This is only achievable through the reorganisation of the joint system.
Now I am not saying that you shouldn’t train your core to be stable, but I am suggesting that it should not be at the cost of the spine’s ability to move. If we can become more stable by virtue of focussing on our body parts and re-educating them in how to move rather than endless hours of sitting on a swiss ball and contracting our TVA in an ability to be still, we may begin to access freer states of movement in our whole body and relieve pressure on the spine.
As an alternative to stabilising the spine then, we could consider mobilising it.
In my book What The Foot? I wrote about a spinal gyroscope which highlights the three degrees of freedom available to the whole spinal column. This essentially means that the spine moves in three planes of motion and has six directions in which to move – two directions in each plane: the six movements are flexion and extension (sagittal plane), side bending to both sides (frontal plane) and rotation to both sides (transverse). To stabilise your spine is to attempt to eliminate these movements rather than promote them. What if promoting movement in each of these six directions is the thing that makes your spine more stable, free from compromise and gives access to beneficial movement to surrounding structures and muscles?
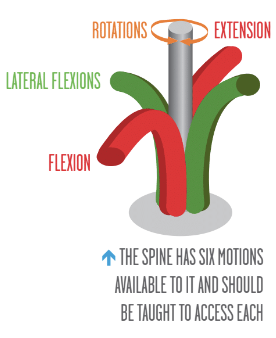
If you feel your COM is not dead Center in your BOS then I can pretty much guarantee that you will have more flexion than extension, or extension than flexion; more side bend to one side than the other and more rotation to one side than the other. This is the very nature of imbalance…. and will not be cured by stabilising the spine. Ironically to be lacking of these movements is to have poor spinal posture as well – so all you would be doing by stabilising your spine is locking that poor posture into place!
Exploring your spinal gyroscope is key to mobilising your spine. Each spinal position communicates movement potential to the rest of the body. This is where it becomes important to educate the rest of the body to get good at following along with the new movement. What if you also had access to information such as “If my spine moves this way, what would it mean for this foot, my knee and also my pelvis” and could you work them all together in one simple movement? Well, quite frankly that is the goal.
Your spinal health is reflected in how well your foot and leg communicate movement upwards in your body and how well your shoulders communicate movement back down into the body as well.
Is your back moving too much due to having feet that lack movement? Is your back unable to move due to how you hold your COM inside your BOS? Is your painful back not the problem but you keep treating it anyway? Without addressing each of these factors, you could end up dealing with your back pain for a much longer time than necessary.
If your BOS has adjusted to hold your COM inside it, what caused your COM to adjust in the first place?
When it comes to deciding what to do with pain, you can literally only do one of two things. We seem to unconsciously move towards our pain or away from it. This is why in our programmes we always ask you to consider your injury history. Would you want to stand on the leg you have broken in the past? Or consciously bear more weight on that ankle that you are always going over? A simple shift of the pelvis away from previous damage is enough to alter how you stand in your base and place pressure on the spine which could lead to a future uncomfortable outcome.
What about a broken arm as a kid? It’s not unusual to see people shift a ribcage away from the arm or to draw the pelvis towards the arm in order to carry it in a protective way; the influence of this is also enough to place future pressure on the spine.
Shoulder injuries? Again, some people lift them up to protect them, others let them just hang out, while again drawing on the spine to alter its shape to manage the injury. And what about head impacts? Can you see how awkwardly holding your skull has a direct influence on the spine as well? This could be from head impacts and concussions.
Forget injury history now for a second, think about posture. Adaptations to sitting, using a mouse, rolling one shoulder forward persistently is enough to affect your feet. It’s all worth paying attention to in the pursuit to end chronic back problems.
I always encourage both practitioners and patients alike to pay attention to their injury history and movement habits. It’s all relevant until it can be ruled out. People will give you the big stuff… but it could equally be the small stuff. A sure fire rule of thumb is often (but not always the case) that where it hurts is probably not where the problem truly is.
My Back Pain 101?
Don’t stabilise. Mobilise.
Assess. Don’t guess.
So, for instance, if I damaged my right ankle and shifted my weight left away from it putting increased pressure and reliance on my left leg, which then exploded while skiing and then required surgery. Where do I move my mass now? With a left foot now more pronated than right which remains stuck in the multiple ankle inversions, my pelvis takes a rotation toward the right foot. Later a dislocated shoulder pulled my ribcage to both rotate and side bend to the right. Add the jaw on top of that which occurred in an abrupt right side bend and left rotation of my skull and the impact of these injuries (there are plenty more but these are the big guns) all influencing movement above and below. What a mess I hear you cry! My back was literally getting it from all directions, above and below.
Compromised movement does one of two things: it requires movement elsewhere in excess or shuts movement down. None of which is useful for a joint’s ability to be centred and have equal access to its ranges in all dimensions. Once I stopped looking for answers for my back and began diligent work on my injured parts to re-learn inherent unconscious movement patterns over time it began to take the pressure off my back.
Back pain doesn’t necessarily need treating per se. All of the parts that have ceased to move will need re-educating to move well giving permission for the body to reorganise itself and take pressure off your back resulting in less low back pain.
What’s your story? Have you thought about it? I guarantee it adds up to who you are and how you move today.
Your back has a requirement to be able to do a handful of simple movements. That’s it. The spinal gyroscope. All it really needs is for the surrounding structures to play ball. If the pelvis which connects with the spine is limited in motion, we should pay attention to what encorauges motion at the pelvis. We know that each leg has a direct impact on that pelvis and that if they are different to each other then the pelvis will move in an imbalanced way and compromise the spine’s movement.
Our online education programmes help you to understand the patterns required in both legs for efficient and optimal movement. My Flow Motion ModelTM is a model that describes how our whole body moves as a unit through the gait cycle, considerate of all of it’s parts and how they communicate together. It describes how these movements come together to create a flowing gait cycle. If our spinal movement is limited thanks to changes in say a foot, then it will become clear in the gait cycle providing you know what you are looking for.
The FMM gives a clear description of the timings and movement of not only each bone and joint but paints a picture of how they all come together to create effortless and efficient shapes of movement necessary to be successful at each moment in each foot step.
We can use our knowledge of how joints function and how they team up together in the phases of movement to begin to re-educate the whole body. As each joint finds centre and is able to access its own movement potential, giving permission to the joint next in line to move cleanly as well, you receive the benefits of postural alignment, effortless movement and efficiency in your overall movement patterns. Optimal alignment is when no joint is compromised, neither open nor closed, pinching or gapped, where each muscle is at resting length, neither too long nor too short, where all parts of the body are free to do their thing. No compromise to the arterial or venous system, to the nervous system, to the organ systems… ultimately creating an environment for overall healing. I have always said at Anatomy in Motion – AiM – we let the body do the healing but first we must create an environment for that to be possible. My Wake Your Body Up programme gives you the opportunity to begin this journey now and my closed chain courses give you the opportunity to learn how to use it and apply it.
Finally as I began this series on a personal note, I shall end it on a personal note…. I no longer have back pain. None. It’s something I haven’t worried about for over fifteen years. As a result, I feel younger, healthier and more physically able than at any time in my younger years and I do not believe it’s ever too late for anybody to start.
Continue Your Journey
👣 Download the Free 7-steps to take ownership of your body. Access the free ebook here
👣 Get started with our self-assessment programmes for Everyone.
👣 To learn the AiM methodology as a practitioner or to support your self-assessment programmes please check out our online Educational courses

One Comment
Awesome read, as always!